Chronic Kidney Disease (CKD)
Information for Swan Medical Group patients
What is Chronic Kidney Diseases (CKD)?
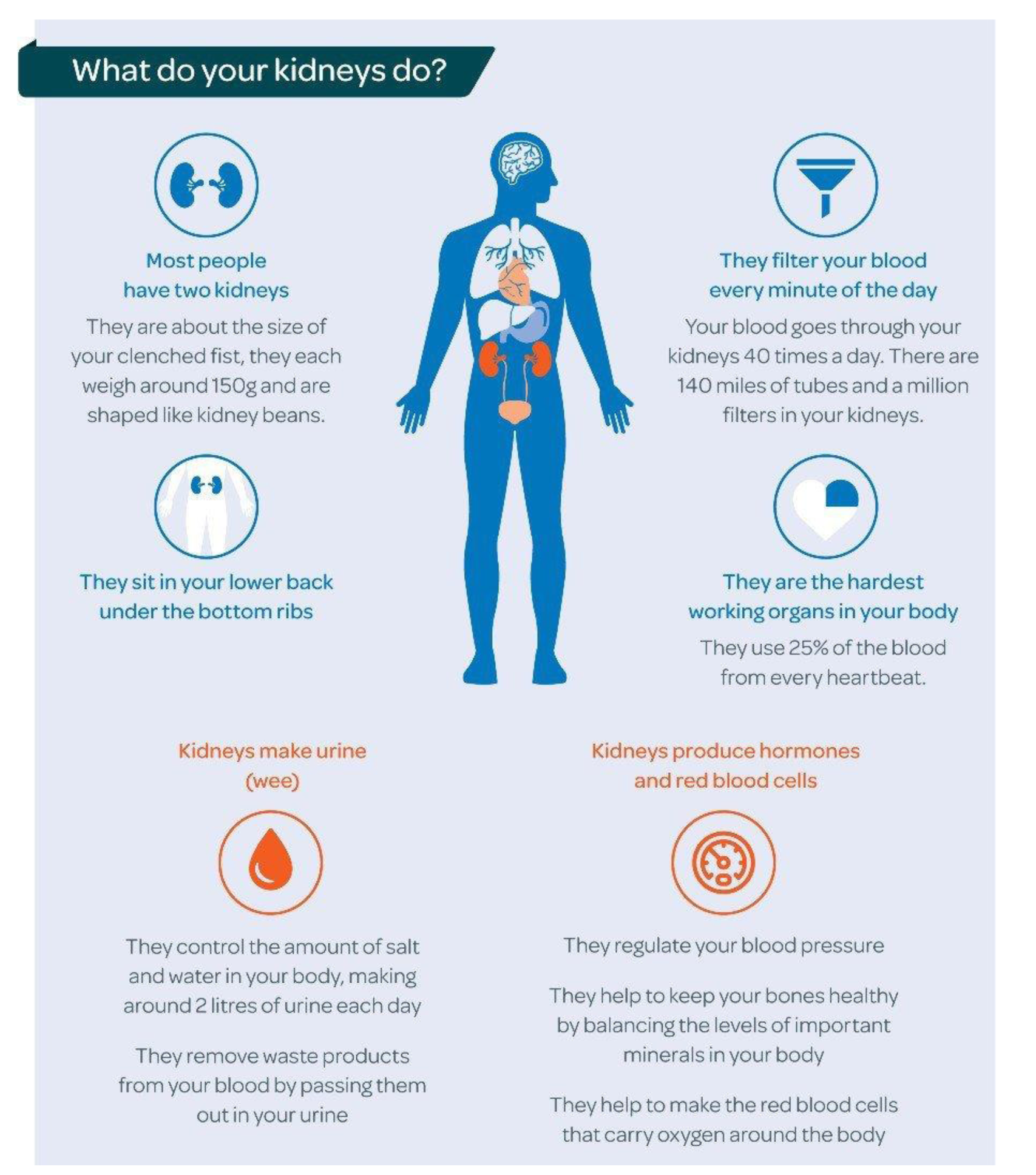
Chronic kidney disease (CKD) is common: around one in 10 people are affected. A diagnosis of chronic kidney disease (CKD) means that your kidneys do not work as well as they should. The term ‘chronic’ means that it is a long-term condition. It does not mean that the condition is severe. Most people with CKD have very mild or no symptoms and are managed long term by their GP.
If you have CKD, your kidneys do not work as well as they should. Damage to your kidneys’ filter system lets blood and protein leak into your urine. Waste products can start to build up in your body as your kidneys can’t remove them properly.
“The good news about being diagnosed early is that we can slow further damage with a combination of highly effective new drug treatments and diet and lifestyle changes. Most people with CKD are able to live full and active lives and feel well.”
How is CKD diagnosed?
CKD is usually diagnosed by blood and urine tests. You may have these tests as part of a routine check-up at your GP surgery or because you are at increased risk of developing CKD because you have other conditions such as diabetes, high blood pressure or heart disease, or a family history of kidney disease.
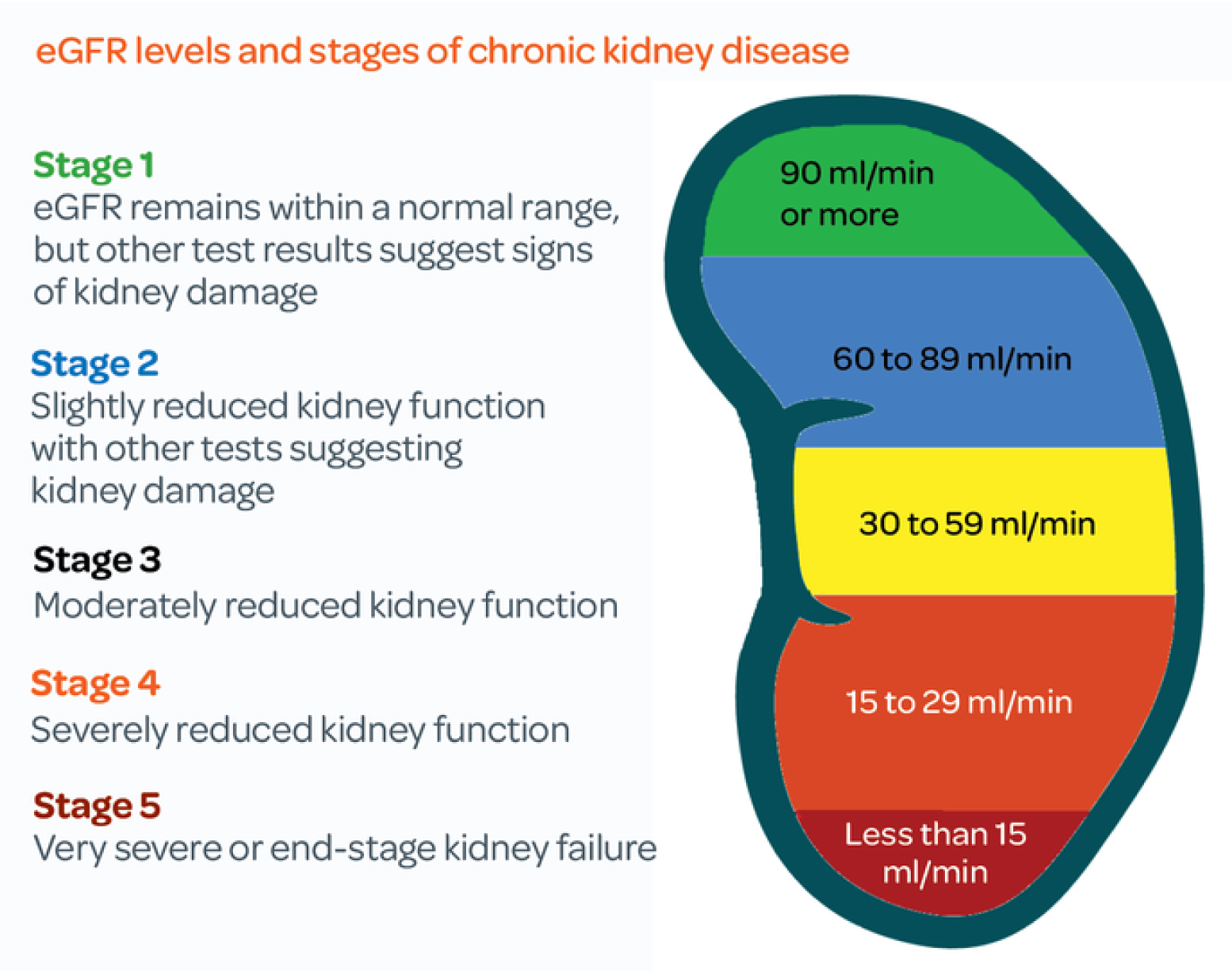
Your doctor, nurse, or health care assistant will carry out a blood test that measures levels of a waste product called creatinine in your blood. They look at the results of this, along with your age, size, ethnic group and gender, to calculate how much waste your kidneys are filtering every minute. The calculation is called your estimated glomerular filtration rate, usually shortened to eGFR. Healthy kidneys should be able to filter more than 90ml/min. To get a fuller picture of your kidney function, doctors will also carry out tests on your urine to look for blood and protein, which can be present if your kidneys aren’t working properly.
CKD is then categorised into FIVE “stages” based on these blood & urine test results. The five stages of CKD range from being at risk (stage 1) through to kidney failure (stage 5). But only around 1 in 100 people with CKD ends up with kidney failure. Most people with CKD Stages 1 – 3 manage the condition themselves with support from their GP. With treatment and lifestyle changes, lots of people stay stable and their CKD doesn’t get worse.
How did I get CKD?
Several factors can affect whether you’ll develop CKD. These include:
- Ageing: The rate at which blood passes through the blood vessels in the kidney each minute drops as you get older as a normal part of ageing. CKD can happen at any age, but kidney function begins to fall by approximately 1 per cent per year after the age of 40. However, your kidney function may never fall as low as the threshold to be classed as CKD.
- High blood pressure: High blood pressure (hypertension) can constrict and narrow blood vessels in the kidneys, causing damage
- Diabetes: Diabetes that isn’t well-controlled can damage blood vessels in the kidneys. This can lead to high blood pressure, which can further damage the kidneys.
- Genetics: Some people are more prone to CKD due to their genes. Some may have inherited kidney diseases, such as polycystic kidneys, but for other people it is a combination of different factors that put them at risk
- Autoimmune diseases: Some autoimmune conditions, such as lupus can increase the likelihood of developing CKD. We don’t fully understand why
- Lifestyle factors: Some lifestyle factors, such as being overweight, can put more pressure on the kidneys and they have to work overtime.
How is CKD treated?
We can’t reverse kidney damage that has already happened; however, we can help stop it getting any worse with drug treatments and lifestyle changes.
If you have mild CKD (stages one to three) and your kidney function is stable, you will be monitored by your GP practice.
What will my GP do?
You will have annual checks with your GP, or practice nurse, to monitor your condition and overall health. At each visit you will have your weight and blood pressure measured and a sample of your urine will be checked for signs of blood, protein or infection. You will have a blood test to measure your kidney function and check for signs of anaemia. Your healthcare professional will discuss any symptoms you may be having and whether any treatment is needed. You will be screened for other conditions, like Diabetes, Hypertension (high blood pressure), and high cholesterol, as managing these conditions will improve your kidney health in the long term.
Some people may have more frequent monitoring if they have recently been unwell or admitted to hospital, if they are changing or starting new medication, or if they have had a recent decline in kidney function.
Medication
You may need to take medication to reduce your blood pressure or control your diabetes. These conditions can make your CKD worse if uncontrolled as they damage blood vessels in the kidneys.
- For anyone with CKD stage 3-5, a statin is recommended. This should be discussed with your GP, or a pharmacist. This is recommended even if your cholesterol level is ok, or your QRISK score (risk of having a heart attack or stroke in 10 years) is ok. Reducing cholesterol protects the blood vessels in the kidney, and statins also have anti-inflammatory effects which are kidney-protective.
- NICE recommends that people with CKD who either have diabetes, or protein in their urine are prescribed SGLT2 inhibitor drugs which can help to slow down CKD progression and have also been shown to reduce your chances of having a heart attack or stroke. In addition, those with diabetes already on an SGLT2 inhibitor can sometimes be offered an additional drug called finerenone (a non-steroidal mineralocorticoid receptor).
If you have Severe CKD (stages four to five) you will be referred to a specialist (nephrologist). Your specialist will give you support and advice to help you understand your treatment options, which may include dialysis, a kidney transplant or conservative care. Some foods that are high in salt, potassium and phosphate can be harmful to your kidneys. Your kidney team will tell you if you need to lower the amount of potassium in your diet. A dietitian can give you specialist advice on how you can adapt your diet if needed.
What can I do to keep healthy?
- Eat a healthy balanced diet.
- Take regular exercise. This can be as simple as increasing the amount of walking that you do each day. Doing any amount of exercise is better than doing none. Your GP can give you advice about how to exercise safely.
- Give up smoking. Your GP can help you with this.
- Give up or cut down on your alcohol intake.
- Keep up to date with your vaccinations. When you have kidney disease, you are more likely to get other illnesses and take longer to recover. This can make your kidney function worse, so it is important to get treatment early. Ask your GP about having flu, pneumonia and Covid-19 vaccinations.
- Check your blood pressure regularly. Your GP can teach you how to do this yourself at home.
- Some over-the-counter and prescription medicines can make your kidney disease worse. Always tell your doctor and pharmacist that you have kidney disease and check that the medication you are given is safe to take.
- Do not stop any medication without taking medical advice.
For more detailed healthy eating and lifestyle advice: https://kidneycareuk.org/get-support/healthy-diet-support/healthy-eating-and-lifestyle-for-your-kidneys/
What if I have more questions?
You can contact us at Swan Medical Group where one of our expert team of GPs, pharmacists, and advanced nurse practitioners will be able to help you.
You can also find out more information online, but please make sure to only visit trusted sites with good quality information, such as the NHS website and Kidney Care UK
https://www.nhs.uk/conditions/kidney-disease/
https://kidneycareuk.org/
https://www.kidney.org.uk/chronic-kidney-disease
https://www.kidneyresearchuk.org/conditions-symptoms/chronic-kidney-disease/

