Ankle Pain
The foot and ankle form a complex system which consists of 28 bones, 33 joints, 112 ligaments, controlled by 34 muscles.
The ankle joint is comprised of 3 parts: the tibia and fibula (shin bones) meeting the talus (foot). The ankle works with the foot to provide a mobile platform to help stabilise the lower limp while walking and standing, but also as a rigid lever to propel you forward while engage in activity
What are the common causes of ankle pain?
Common causes of musculoskeletal related pains tend to originate from bones, ligaments, tendons and muscles. These symptoms tend to settle with time and good self-management.
These pains may be a result of an acute injury or a flare up of a long standing issue. Simple advice is keep active and keep moving, it will often settle with time.
Click on the following information to find out about common conditions related with ankle pain.
Common conditions of the Ankle
See below for the common signs and symptoms with a link to the MSK Matters page on how best to manage it.

Early management of sprains and strains
Click here for more information on early management of sprains and strains
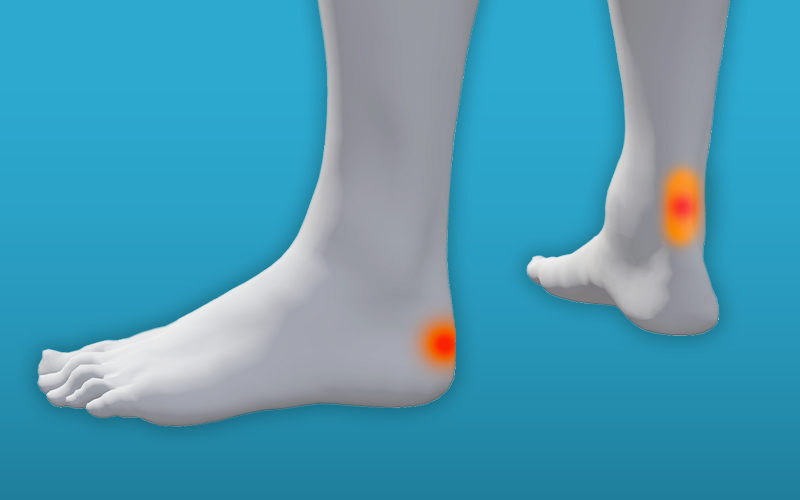
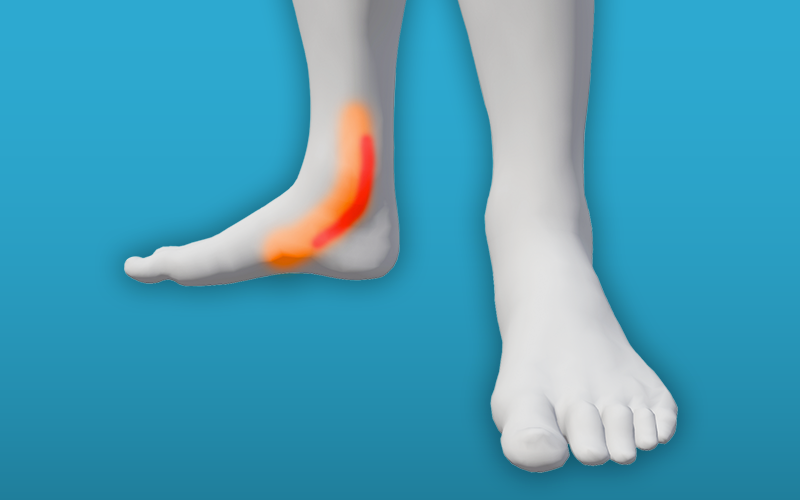
Achilles tendinopathy
- Pain is at the back of the calf or ankle
- Pain is often in the middle of the tendon or can be at the end of the tendon where is attaches
- You may notice a tender, warm, red lump at the back of your heel or on the tendon itself
- Pain is often worse on the first few steps in the morning
- The tendon may feel stiff after rest
- The tendon may feel tighter than that of the opposite foo
- Onset is often after a sudden change in activity
Tibialis posterior tendinopathy
- Pain on the inside of the ankle
- There can be swelling on the inside of the ankle
- If there is a significant injury to the tendon it can lead to a flat foot
- There can be weakness to the tibialis posterior muscle
- Pain is often present when doing weight bearing activities such as walking or running
- Pain can be worse when walking barefoot
Click here for more information on tibialis posterior tendinopathy


Peroneal tendinopathy
- Pain is on the outside of the ankle
- There can be swelling on the outside of the ankle
- Often associated with an injury such as an ankle sprain
- It can be cause by an overload or accompanied with poor fitting shoe
Osteoarthritis of the ankle
- Pain can be sharp or an ache all around the ankle
- Often a gradual onset of pain and joint restriction
- Stiffness first thing in the morning for 30 minutes or less
- Stiffness after a period of rest
- Pain often on weight bearing activities
- Noise or crepitus on moving the joint
Click here for more information on osteoarthritis of the ankle
Footwear
Footwear plays a large role in the development and prevention of many foot and ankle conditions. In general wearing shoes that fit properly will prevent future problems, help you to have less foot pain and allow you to continue to do your normal day-to-day activities. Here is some general advice on managing your footwear.
How to choose the best shoe?

Get your feet measured as your shoe size can change and it is more important how the shoe feels rather than its size number.
A low heeled shoe is usually better and shoes with laces or straps allow greater adjustment particularly if the feet swell. The heel should be not higher than 4cm (1 ½ “)
Shoes that have prominent seams could rub on the skin of your foot and cause irritation so look for shoes with a smooth lining. Also, shoes made of natural materials will shape around your foot and are breathable.
The front of the shoe, known as the toe box, must be foot shaped and allow enough room for your toes. Narrow shoes can pinch the toes causing pressure and pain. The recommendation is a thumbs width from the end of your longest to the end of the shoe and room to touch the roof the shoe with the great toe.
When buying new shoes, try to do this later in the day as this is when our feet are slightly more swollen in the late afternoon. Try on new shoes with the socks that you normally wear and any insoles that you may use. This will ensure that you get the right sized shoes.
Walk around the shop to make sure the shoes are comfortable. They should be comfortable from when you first try them on. Wear new shoes indoors to start with to allow for the materials to expand to your foot shape. This can reduce any risk of rubbing leading to blistering.
Fastenings on the shoes should ideally be lace ups or a strap that hold the foot securely in place across the midfoot.
If you have arthritis of the foot or ankle, shoes that are stiff will help limit the painful movement. Laces up boots are usually very helpful for this. If you can bend your shoe in half it will not support your foot properly.
It would be preferable in the shoe had an insole that is removable in case an orthotic or padding is ever needed. This will allow for the extra space needed for both the feet and the insoles.
Good footwear and getting foot pain managed is particularly important if you have delicate skin or altered sensation in your feet. Good footwear can prevent skin ulcers, blisters and the build-up of hard skin.
If you do have delicate skin or altered sensation, make sure you check your feet before and after you have worn shoes. This is best done by using your hands, check any areas of your foot that may have rubbed against the material of the shoe.
Avoiding ankle pain
Lifestyle
Smoking, being physically inactive and overweight can all increase the risk of developing musculoskeletal damage. These lifestyle factors are also closely linked with long-term diseases such as heart problems and diabetes which can result in delayed and poor healing.
Footwear
Modifications to your footwear with the use of simple insoles and supportive shoes or trainers will help with the management of foot pain.
See the footwear section for further advice.
Activity
Regular physical activity can reduce the risk of ankle problems by strengthening the supporting muscles.
Regular weight bearing activity such as walking can help to prevent osteoporosis – the pulling and tugging on bones by muscles during exercise helps to maintain bone strength.
Musculoskeletal pain can take around 6 weeks to recover. A modification or reduction in activity can sometimes help. If your pain worsens considerably or does not improve after 6-8 weeks please see your GP.
Keep active and avoid a sedentary lifestyle. Aim to do at least 30 minutes of moderate physical activity most days of the week including exercises which encourage flexibility and strength. Find something you enjoy!
Weight
Being overweight or obese can cause musculoskeletal pain and mobility problems as well as anxiety and depression. Increased weight will add pressure on the lower legs and feet, thereby increasing symptoms in these areas.
Keeping active and eating a healthy, balanced diet will help reduce weight loss. Reducing your sugar and fat content and eating smaller sized portions will help with this.
Smoking
Smoking affects the circulation and therefore slows and impairs healing particularly in the lower leg and feet.
You are 4 times more likely to quit smoking with support from Stop Smoking Services than by going it alone.
Is your pain coming from somewhere else?
Pain in the foot and ankle can be as a result of pain elsewhere in the body; this can be the lower back, hip or the knee. Commonly this is known as referred pain. Your physiotherapist or GP can advise on how to manage this with advice and exercises.
When to seek medical advice
The above advice can help you to manage your condition at home. The majority of musculoskeletal conditions get better within six to eight weeks although sometimes they can persist for longer but this doesn’t mean there is something seriously wrong.
However, rarely, musculoskeletal symptoms can be caused by something more serious and it is important for you to know when to seek advice. We would advise if you experience any of the following you should seek the advice of you GP.
- the pain you are experiencing is getting worse rather than better despite following the self-management guidance above for the condition in the time frame expected
- symptoms have not been significantly helped by a trial of medication as expected
- you feel unwell and suffer symptom such as fever, night sweats or weight loss
- you experience pain at night, possibly worse than during the day that prevents you from sleeping due to increasing pain and/or difficulty lying flat.
- you experience a change in your ability to walk including balance problems or weakness/heaviness in your legs
- you develop a hot and swollen joint for no apparent reason
- early morning stiffness, lasting for longer than 30 minutes
