Ankle pain – Achilles Tendon pain
What is it?
The Achilles tendon is the largest and strongest tendon in the body and is the combined tendon of the two largest calf muscles, the gastrocnemius and soleus. It is situated at the back of the ankle and can be felt as a cord that connects the muscles of the calf to the heel bone.
When the tendon contracts, it has the effect of pointing the foot down which is important for running, walking, jumping and stair climbing.
Despite being the strongest tendon in the body, it can sometimes be overloaded, causing discomfort and even pain.

Achilles tendinopathy causes are not fully understood however there are many factors that can increase the risk of developing it:
- Weak or tight calf muscles
- Stiff ankle joints
- Weight gain or being overweight
- Training problems such as lack of pacing, increasing intensity, distance or time of training too quicky. Lack of variation in training regimes can also cause overuse and discomfort.
- Old or inappropriate footwear
- Some rheumatological conditions or diabetes
Common symptoms
You may notice a tender, warm, red lump at the back of your heel or on the tendon itself. The tendon may feel tighter than that of the opposite foot.
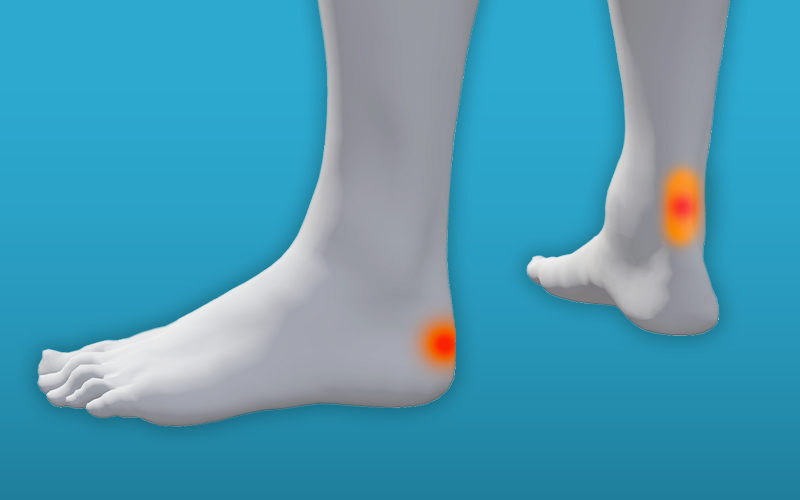
If the pain you are feeling is on or around the mid-point of the tendon this is known as non-insertional Achilles tendinopathy. If your pain is around the heel where the tendon attaches this is known as insertional Achilles tendinopathy. The picture is annotated to the right highlights these 2 areas of pain.
The area of tendon may feel stiff for a short while in the morning (especially going downstairs), but settle when you start walking.
Pain can occur when you have walked or run for a period of time and gets worse the more you walk or run. For some people however, they are able to exercise through the initial pain but then worsen again after rest.

How to manage it
The Achilles tendon becomes painful and swollen because it has been overloaded, This means it is unable to adapt with the load placed upon it. It is important to reduce the load on the tendon initially. Total rest, however, can make matters worse, causing weakness.
Activity modification
Modifying your daily activities by reducing the activity that has caused your problem will help. For example, some runners will find that not running for the first six weeks of starting the Achilles strengthening exercises should help. After this time running can be restarted gradually.
In the meantime, switching to other exercise types, where weight through the heel is reduced such as swimming and cycling may help to maintain your cardiovascular fitness level.
Exercise
The most effective treatment is to perform a training programme which strengthens the tendon by loading it and therefore allowing rapid healing.
These exercises are often very uncomfortable to start with, but be reassured that this will get easier and you will not be doing any harm. This treatment plan may take around three months to make a difference, so don’t give up too early.
Please consult a GP or physiotherapist if you are unsure how to perform your exercises, or if symptoms do not settle or worsen after 12 weeks.
Achilles tendinopathy exercises
Sitting heel raises
In sitting, feet flat on the floor.
Slowly lift your heels and hold for 2 seconds, slowly lower down to the floor.
Repeat 10 times rest for 1 minute. Repeat 3 times.

Standing heel raises
When sitting heel raises are comfortable progress to standing heel raise
Stand with support, feet flat on the floor, slowly lift your heels off the floor and hold for 2 seconds, slowly lower down to the floor.
Repeat 10 times, rest for 1 minute and repeat 3 times.

Eccentric training
This means exercising your muscle while they lengthen, this helps the strengthen your Achilles tendon and your calf muscles. It can help you recover from Achilles tendinopathy.
Please note that there is a slight difference to the non-insertional and insertional Achilles tendinopathy eccentric exercises.
The following exercise should be done over a 12 week period.
- Stand on a step for non-insertional Achilles tendinopathy, or stand on the floor for insertional Achilles tendinopathy, use a rail for support if needed
- Slowly raise up onto both feet
- Transfer all your weight to your affected leg and slowly lower down to the step or the floor
- Repeat 15 times, rest for 1 minute and repeat 3 times

As your pain improves, you can progress the exercise above. Progress gradually and only if your symptoms allow this.
Progression:
- drop your heel below the level of the step,
- increase the speed of the exercise,
- add weights
Footwear
This also plays a big part in the prevention of Achilles pain. Make sure that the shoes you have are supportive and appropriate for the activities you use them for. They should fit properly are not be worn out (you should consider renewing your trainers after about 500 miles of use).
See the footwear section for more advice.
Ice Therapy
Some people find using ice on the hot, swollen area can help.
Use a damp cloth containing an icepack (or bag of frozen peas) on the painful area to help numb the pain. Apply it for up to 20 minutes, up to three times a day.
- People should be cautious using these treatments if they have altered skin sensation or circulatory problems.
- Check the skin regularly during and after the ice pack application
- Stop if there is excessive pain, numbness or tingling
- Do not put ice directly on to the skin as this may cause a burn.
Simple painkillers
Painkillers like paracetamol will ease the pain, but need to be taken regularly in order to control the pain. Always follow the instructions on the packet.
Anti-inflammatories like ibuprofen can help with swelling, and therefore help you move more freely. Topical (applied directly on the affected body area) anti-inflammatories are recommended initially. Follow the instructions on the packet and discuss using them safely with a pharmacist, especially if you have any underlying health conditions
However, you should not take ibuprofen for 48 hours after an initial injury as it may slow down healing.
Up to date guidelines can be found on the NHS website:
Other medicines can help to reduce inflammation, swelling and pain. You should discuss this with your GP if the simple pain relief advice does not help or if you are needing to take ibuprofen for more than 10 days.
Physiotherapy
If you find that you are not improving, some advice or treatment from a physiotherapist can be helpful in managing Achilles tendinopathy. Click here to self-refer to a physiotherapist.
How to prevent and manage future flare ups of pain
You can reduce your risk of developing Achilles pain by performing strengthening exercises regularly. It takes time for your body to get used to a new activity and tendons take longer than muscles to adapt. So, it’s important to pace yourself and if in doubt, take advice from a physiotherapist.
